 “Am I transgender?” This is a question that all trans people have faced at some point, or at many points, becoming the focus of self-reflection and personal exploration however brief or protracted. Among the community, this line of inquiry has inspired a number of mental exercises such as considering how you might feel if you were told you were indeed transgender (or not), whether you would press a button to become another sex instantly, and other scenarios meant to illuminate feelings and desires about one’s gender. Such informal and open-ended processes can be useful to varying degrees for different individuals; for instance, when I created the single-page website AmITransgender.com which always displayed the word “yes”, some trans and gender-questioning people found this affirmation to be valuable in thinking about their gender, while others saw it as a flippant and unhelpful response to a serious question.
“Am I transgender?” This is a question that all trans people have faced at some point, or at many points, becoming the focus of self-reflection and personal exploration however brief or protracted. Among the community, this line of inquiry has inspired a number of mental exercises such as considering how you might feel if you were told you were indeed transgender (or not), whether you would press a button to become another sex instantly, and other scenarios meant to illuminate feelings and desires about one’s gender. Such informal and open-ended processes can be useful to varying degrees for different individuals; for instance, when I created the single-page website AmITransgender.com which always displayed the word “yes”, some trans and gender-questioning people found this affirmation to be valuable in thinking about their gender, while others saw it as a flippant and unhelpful response to a serious question.
Meanwhile, anti-trans activists have long complained about the lack of any kind of test for a definitive marker that allows the accurate identification of transness or gender dysphoria. Endocrinologist Dr. Michael Laidlaw has claimed that there is “no objective test to diagnose” a person as transgender before gender-affirming medical treatments are pursued; a detransitioned cis woman by the name of Stella has asserted that trans youth can simply “walk into the doctor’s office, tell them you have a certain condition, which has no objective test … and receive life-altering medications on your say-so”. These individuals seem to regard the diagnosis of gender dysphoria as only being legitimate if it is based on some kind of physical assessment of one simple and unambiguous trait, akin to PTC taste test strips or a pathologist’s analysis of a tissue biopsy to identify cancer. But not all medical assessments make use of this approach – there is no biologically-based test for a definitive physical sign of depression, and the “gold standard” for assessing depression is a questionnaire. This does not therefore mean that depression is not a real condition, or that it is necessary to develop a more “objective test” before providing treatment for depression.
Existing in the midst of all this are a number of inventories designed by clinicians and researchers to assess gender-dysphoric symptoms and detect the presence of gender dysphoria. One of these instruments, the Gender Identity/Gender Dysphoria Questionnaire for Adolescents and Adults (GIDYQ-AA), was found to correctly identify the presence of gender dysphoria (sensitivity) in 90.4% of patients who were receiving treatment at a gender clinic and correctly identify the absence of gender dysphoria (specificity) in 99.7% who were not gender-dysphoric (Deogracias et al., 2007). Whether this qualifies as sufficiently “objective” to satisfy detractors is uncertain, though it’s questionable whether anything would.
Another inventory, the Utrecht Gender Dysphoria Scale (UGDS), was developed in the Netherlands in the mid-1990s to assess the first cohort of trans adolescents to receive early treatment with puberty blockers (Cohen-Kettenis & van Goozen, 1997), and was found to have a sensitivity of 88.3% and specificity of 99.5% for those assigned male and a sensitivity of 98.5% and specificity of 97.9% for those assigned female (Steensma et al., 2013).
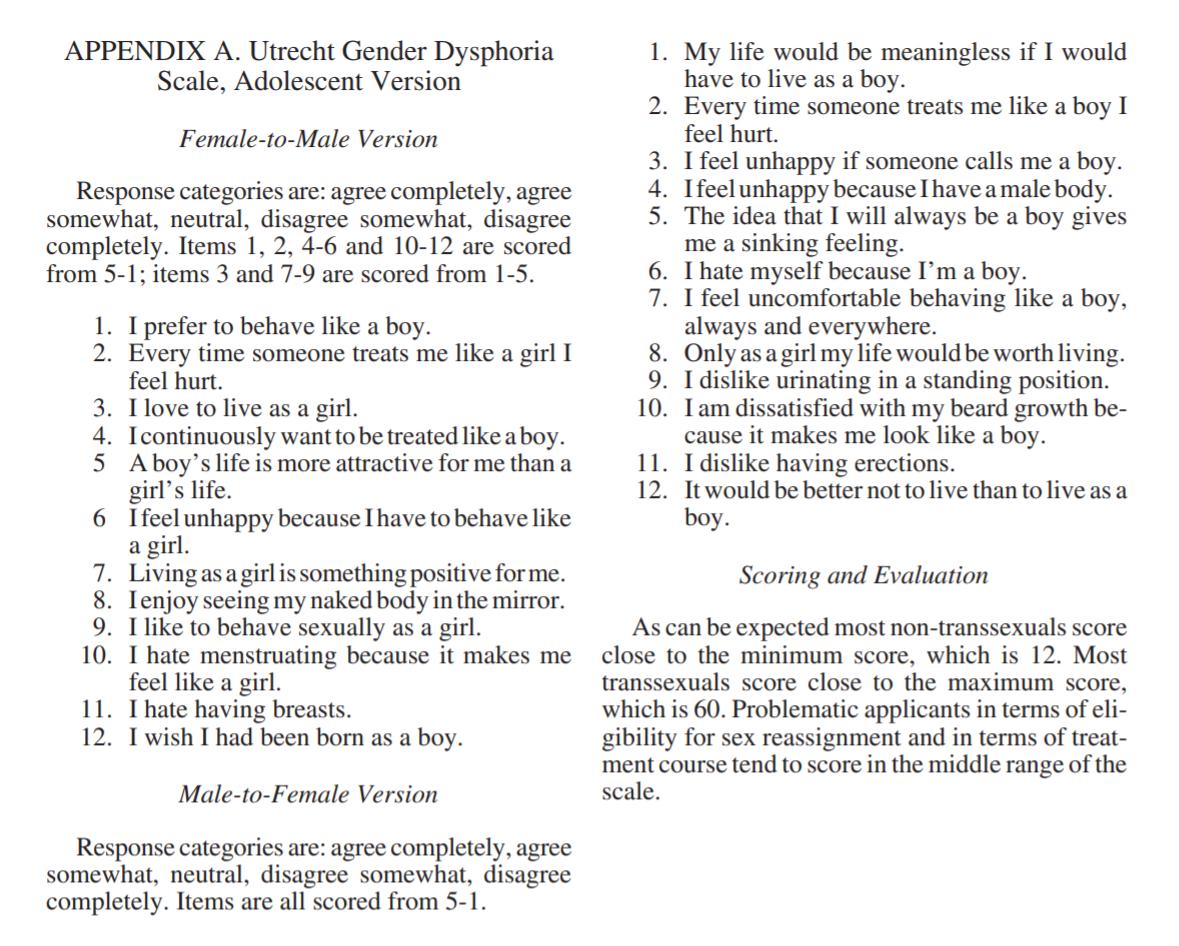
“Clinical Management of Gender Dysphoria in Adolescents” (de Vries, Cohen-Kettenis, & Delemarre-van de Waal, 2006)
One persisting issue with these inventories is that they largely do not account for nonbinary experiences of gender dysphoria, instead defining gender dysphoria in terms of aversion toward one assigned binary sex and affinity with another binary sex. With growing awareness of nonbinary gender identities, this deficiency becomes increasingly troublesome: a trans person can experience gender dysphoria without necessarily identifying with or desiring the typical features of the “opposite” sex, meaning that the questions in these inventories could be inapplicable or produce less accurate results in the case of nonbinary trans people. In a previous study, trans people were asked to rate how well the UGDS and GIDYQ-AA questionnaires reflected their own experience of gender dysphoria; nonbinary and agender trans people gave both inventories a lower rating than transfeminine and transmasculine respondents (Galupo & Pulice-Farrow, 2019).
A new version of the UGDS seeks to remedy this shortcoming: the Utrecht Gender Dysphoria Scale – Gender Spectrum (UGDS-GS) (McGuire et al., 2020). This inventory was developed by researchers who designed the original UGDS, as well as others who designed the recent Genderqueer Identity Scale (GQI), which focused specifically on experiences of and identification with a nonbinary gender. Unlike the original 12-question UGDS with separate versions for those assigned male or female, the 18-question UGDS-GS revision is designed to be suitable for assessing clinically significant gender dysphoria in all trans or gender-questioning people regardless of birth assignment or binary or nonbinary gender identity:
In tests, the UGDS-GS was found to produce an effective measurement of gender dysphoria in binary transgender, nonbinary/genderqueer, and cisgender participants. The need for a nonbinary-inclusive gender dysphoria assessment is particularly urgent given that nonbinary trans people are a substantial proportion of those presenting for evaluation and treatment at gender clinics: Cheung et al. (2020) recently reported that of 895 trans people attending three clinics in Melbourne, Australia, 14.3% were nonbinary, and of those, 53.5% were receiving hormone therapy and 14.1% had already received gender-affirming surgeries. Nonbinary trans people can experience gender dysphoria and may pursue medical transition as part of treatment for gender dysphoria, and the UGDS-GS can help clinicians in assessing and caring for them.
To be sure, questionnaires like the UGDS-GS cannot definitively answer the question of “am I transgender?”, and these are not meant to serve as some kind of PTC taste test strip for dysphoria. These instruments rely on one particular definition of gender dysphoria, and not all trans people experience gender dysphoria or experience it in the same way. Among respondents in Galupo & Pulice-Farrow (2019), only 52.5% said that the GIDYQ-AA effectively captured their experience of gender dysphoria and 54.6% said the original UGDS captured their experience. Deogracias et al. (2007) suggested that the GIDYQ-AA “can be used to identify ‘caseness’ if one wishes to use as a ‘gold standard’ patients referred to a specialized gender identity clinic” – that is, the inventory assesses the extent to which a person’s experience of gender dysphoria is similar to those who have been clinically diagnosed with and received affirming treatment for their gender dysphoria. In a study comparing the original UGDS and GIDYQ-AA, Schneider et al. (2016) pointed out that “it might be possible that the construct of gender dysphoria consists of more components than measured by the instruments”.
These tests are not meant as a final answer, and they’re not meant to constrain your options and possibilities. What they can provide is yet another piece of information that can help to guide you as you continue to explore. ■




