by Zinnia Jones — January 31, 2018
Depersonalization disorder (DPD), also known as depersonalization/derealization syndrome, is a dissociative condition characterized by feelings of “unreality”. These can include emotional numbing or feeling like a robot, a sense of having “no self”, a perceived loss of agency in one’s life, and a lack of spontaneity. Sufferers may experience themselves as separated into an exterior participator who moves about in the world and an interior observer who remarks on this. They may feel that the world around them is lifeless, colorless, or less than real; their life can feel dreamlike or as if they’re separated from the world by a veil or fog. Depersonalization disorder is not a psychotic condition: those experiencing this have an intact grasp of reality; it is the feeling of existence that has taken on these peculiar and unnerving textures (American Psychiatric Association, 2013). The syndrome of chronic depersonalization is typically constant and unremitting, and this highly distressing condition is associated with a number of adverse mental health and social outcomes.
Regardless of the emotional flattening often experienced in depersonalization disorder, the emotional pain of living with depersonalization can be profound and unbearable, and the pervasive sense of existence as being unreal can lead to a total disinvestment from one’s life in the world. Despite its severe impact on sufferers, very few treatments have been found to be effective in treating chronic depersonalization. Numerous approaches have been tried in small studies, including antidepressant medication, opioid antagonists, cognitive-behavioral therapy, mindfulness therapy, biofeedback, and transcranial magnetic stimulation (Hunter, Charlton, & David, 2017).
One of the few pharmacological treatments that has shown some efficacy in clinical studies and individual case reports is the combination of serotonergic antidepressants, such as SSRIs or SNRIs, with the anticonvulsant and mood stabilizer lamotrigine (Lamictal). This approach is based on the ability of some dissociative drugs, particularly ketamine, to induce pronounced symptoms of depersonalization by antagonizing NMDA receptors and stimulating the release of glutamate. Lamotrigine conversely inhibits the release of glutamate, and has been found to attenuate the effects of ketamine, including symptoms of depersonalization and derealization. Clinicians researching and treating depersonalization disorder at the Depersonalisation Research Unit of King’s College London have described lamotrigine as “often our first-line treatment for the condition” (Medford et al., 2005):
Lamotrigine acts at the presynaptic membrane to reduce the release of glutamate, and it has been shown to reverse depersonalisation-related phenomena induced by the N-methyl-D-aspartate (NMDA) receptor antagonist ketamine in healthy individuals (Anand et al, 2000). In the absence of large-scale randomised controlled trials, and in the presence of conflicting published data (see below), the efficacy of lamotrigine (whether as monotherapy or in conjunction with an SSRI) is not yet firmly established, but it is often our first-line treatment for the condition.
Neither lamotrigine alone nor serotonergic antidepressants alone have been shown to be reliably effective in treating depersonalization disorder, but existing data indicates that when used in combination, these medications can produce a marked reduction in symptoms. Sierra (2008) observes:
Such findings suggest that rather than acting on its own, lamotrigine works better as an add-on therapy with SSRI antidepressants. This possibility is not surprising in view of the circumstantial evidence reviewed earlier, which points to an involvement of both serotonergic and glutamatergic mechanisms in depersonalization. If that is indeed the case, it may be that successful pharmacological interventions need to target both neurotransmitter systems.
Clinical studies
Sierra et al. (2001) described a case series of 11 patients with depersonalization disorder, all but one of whom were concurrently taking SSRIs. When treated with lamotrigine as an add-on medication, six of these patients experienced a notable reduction in their symptoms over the course of one month:
Six patients reported subjective beneficial effects ranging from 40% to 80% on a subjective improvement scale. These effects were confirmed by a drop in their PSE [Present State Examination] score and DES [Dissociative Experiences Scale] depersonalization subscale store. The other 5 patients in the sample reported no beneficial effect, and their scores on the outcome measures remained unchanged. None of the patients reported side effects. In all cases, improvement occurred on treatment with lamotrigine doses from 200 to 250 mg/day.
Sierra et al. (2003) conducted a cross-over trial of lamotrigine compared to placebo (lamotrigine then placebo, or placebo then lamotrigine) in a group of nine patients with depersonalization disorder who were not taking any other medications. The study found a null result:
Lamotrigine was not significantly superior to placebo. None of the nine patients was deemed a responder to the lamotrigine arm of the cross-over.
Each phase of the trial lasted 12 weeks, and no patient showed a reduction of more than 12% in their Cambridge Depersonalization Scale (CDS) or PSE scores on lamotrigine compared to their baseline scores.
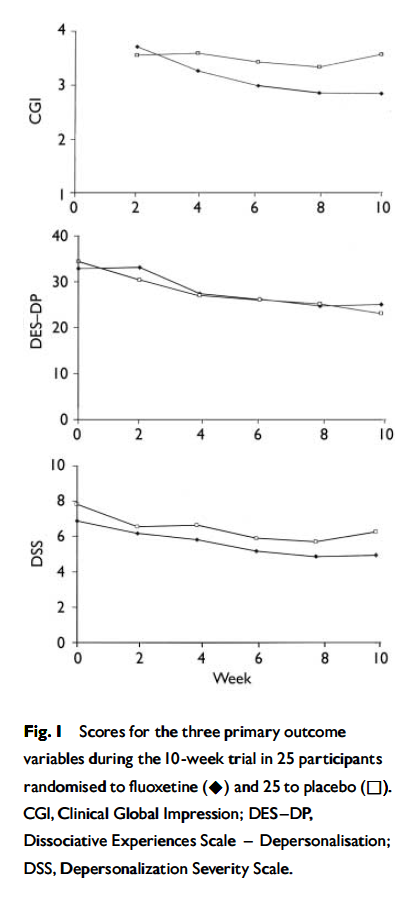
Simeon et al. (2004) compared treatment with the SSRI fluoxetine at 10-60 mg/day to placebo in a group of 50 patients with depersonalization disorder taking no other medications. 37 completed the 10-week study, which did not show a significant difference between fluoxetine treatment and placebo: 24% of the fluoxetine group were considered responders, compared to 20% of the placebo group.
Both clinician-rated and self-rated dissociation scores showed a modest decline in both treatment groups, which was clinically not noteworthy and statistically no different. . . .
Our study suggests that first-line use of serotonin reuptake inhibitors for the treatment of depersonalisation disorder is not indicated, except possibly in selected individuals with troublesome anxiety or depression; in such individuals, improved affective state might result in a somewhat better tolerance of their dissociative symptoms.
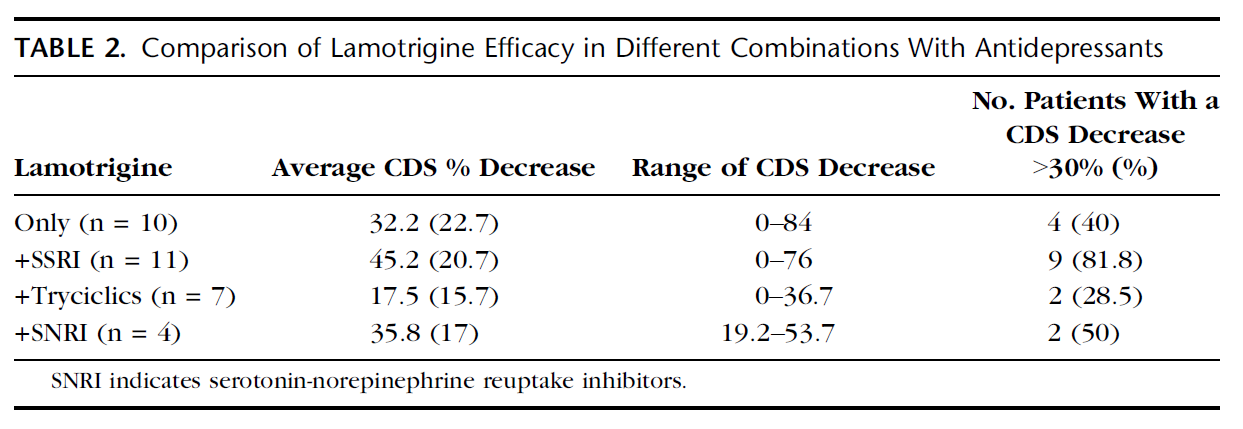
Sierra et al. (2006) presented a case series of 32 patients with depersonalization disorder who had been treated with lamotrigine, most of whom were concurrently taking an antidepressant medication (SSRIs, SNRIs, or tricyclic antidepressants). 56% of patients overall showed a response of a 30% or greater reduction in their CDS score during treatment with lamotrigine, which lasted for an average of 13.7 months. Of those patients taking lamotrigine in combination with an SSRI, 81.8% achieved a reduction of 30% or more in their CDS score, compared with 50% of patients taking an SNRI with lamotrigine and 40% of patients taking lamotrigine alone. Lamotrigine doses ranged from 25 to 600 mg/day, and a greater lamotrigine dose was significantly correlated with a greater decrease in CDS score.
In keeping with the previous study, our findings suggest that, rather than acting on its own, lamotrigine works better as an add-on therapy with SSRI antidepressants. This possibility would not be surprising, in view of the circumstantial evidence reviewed earlier, which points to an involvement of both serotonergic and glutamatergic mechanisms in depersonalization, and previous clinical experience in the use of lamotrigine. If that is indeed the case, it may be that successful pharmacological interventions need to target both neurotransmitter systems. Other conditions for which there is growing evidence of the effectiveness of lamotrigine include post-traumatic stress disorder and borderline personality disorder in which emotional blunting and dissociation are observed, respectively, symptoms which overlap with those seen in DPD.
Case reports
Rosagro-Escámez et al. (2011) describe the case of a patient diagnosed with obsessive-compulsive disorder, borderline personality disorder, and depersonalization disorder. She had previously been treated with sertraline alone and citalopram alone, with “poor response”. Upon commencing combination treatment with sertraline, clomipramine (a tricyclic antidepressant and SNRI), and lamotrigine, the patient experienced a “significant improvement” in her depersonalization.
Salgado et al. (2012) report on the case of a woman with depersonalization disorder who had previously been unsuccessfully treated with risperidone (an atypical antipsychotic) alone and an SSRI alone. She was then treated with venlafaxine (an SNRI) alone, which improved her mood and panic episodes but did not affect her depersonalization symptoms. When lamotrigine was added, she showed “significant improvement in different aspects, such as affect, interpersonal contact and social interaction”, and her symptoms of depersonalization “gradually decreased”. Her CDS score also showed a reduction of 24% following the addition of lamotrigine.
Belli et al. (2014) describe the case of a patient with major depression and depersonalization disorder, who had previously been unsuccessfully treated with SSRIs, SNRIs in combination with atypical antipsychotics, tricyclic antidepressants, and bupropion. She was subsequently prescribed sertraline in combination with lamotrigine, and her symptoms of depression and depersonalization “were markedly improved”.
McEvoy, Anton, & Chisolm (2015) report the case of a patient who developed panic disorder, major depressive disorder, and depersonalization/derealization after taking mefloquine, an antimalarial drug associated with potentially severe psychiatric side effects (Ritchie, Block, & Nevin, 2013). After having his dosage of escitalopram increased, his mood symptoms remitted, but his depersonalization symptoms continued. When lamotrigine was added, this “resulted in decreased intensity and frequency of the depersonalization symptoms to the point that they no longer bothered him.”
Bout et al. (2017) describe the case of a man who experienced the onset of chronic depersonalization following marijuana use. He had previously taken paroxetine, fluoxetine, and olanzapine (an atypical antipsychotic), with no change in his symptoms. After being given a combination of fluoxetine and lamotrigine, his depersonalization symptoms began to abate, with “a significant functional improvement and a marked mitigation of the strange subjective experience”.
References
- American Psychiatric Association. (2013). Depersonalization/derealization disorder. In Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author.
- Belli, H., Akbudak, M., Ural, C., & Aslaner, D. (2014). A case of depersonalization with treatment-resistant depression successfully treated with sertraline-lamotrigine combination. West Indian Medical Journal, 63(1), 115. [Full text]
- Bout, A., Berhili, N., Benbrahim, M., Aalouane, R., & Rammouz, I. (2017). [Lamotrigine in the treatment of resistant depersonalization disorder: a case report]. L’Encéphale. Advance online publication. doi: 10.1016/j.encep.2017.04.003 [Abstract]
- Hunter, E. C. M., Charlton, J., & David, A. S. (2017). Depersonalisation and derealisation: assessment and management. BMJ, 356, j745. [Abstract]
- McEvoy, K., Anton, B., & Chisolm, M. S. (2015). Depersonalization/derealization disorder after exposure to mefloquine. Psychosomatics, 56(1), 98–102. [Abstract]
- Medford, N., Sierra, M., Baker, D., & David, A. S. (2005). Understanding and treating depersonalisation disorder. Advances in Psychiatric Treatment, 11(2), 92–100. [Full text]
- Ritchie, E. C., Block, J., & Nevin, R. L. (2013). Psychiatric side effects of mefloquine: applications to forensic psychiatry. Journal of the American Academy of Psychiatry and the Law, 41(2), 224–235. [Full text]
- Rosagro-Escámez, F., Gutiérrez-Fernández, N., Gómez-Merino, P., de la Vega, I., & Carrasco, J. L. (2011). The efficacy of lamotrigine in a resistant case of depersonalization disorder. Actas Españolas de Psiquiatría, 39(4), 263–266. [Abstract] [Full text]
- Salgado, A., Oliveira, L., Sierra-Siegert, M., & Salgado, J. V. (2012). Depersonalization and derealization syndrome: report on a case study and pharmacological management. Revista Brasileira de Psiquiatria, 34(4), 505–508. [Full text]
- Sierra, M. (2008). Depersonalization disorder: pharmacological approaches. Expert Review of Neurotherapeutics, 8(1), 19–26. [Abstract]
- Sierra, M., Baker, D., Medford, N., Lawrence, E., Patel, M., Phillips, M. L., & David, A. S. (2006). Lamotrigine as an add-on treatment for depersonalization disorder: a retrospective study of 32 cases. Clinical Neuropharmacology, 29(5), 253–258. [Abstract]
- Sierra, M., Phillips, M. L., Ivin, G., Krystal, J., & David, A. S. (2003). A placebo-controlled, cross-over trial of lamotrigine in depersonalization disorder. Journal of Psychopharmacology, 17(1), 103–105. [Abstract]
- Sierra, M., Phillips, M. L., Lambert, M. V., Senior, C., & David, A. S. (2001). Lamotrigine in the treatment of depersonalization disorder. Journal of Clinical Psychiatry, 62(10), 826–827. [Abstract]
- Simeon, D., Guralnik, O., Schmeidler, J., & Knutelska, M. (2004). Fluoxetine therapy in depersonalisation disorder: randomised controlled trial. British Journal of Psychiatry, 185(1), 31–36. [Full text]
Last updated: Jan 31, 2018
Citation: Jones, Z. (2018, January 31). Lamotrigine in combination treatment for depersonalization disorder. Gender Analysis. Retrieved from https://genderanalysis.net