 Puberty blockers are used in the treatment of appropriately diagnosed transgender youth, who wish to avoid developing undesired secondary sex characteristics of their assigned sex but are not yet old enough to commit to the permanent changes of hormone therapy. These medications, which are now administered at hospitals and gender clinics across the United States with the support of several major medical organizations, give an adolescent time to consider whether they want to go on to transition. Crucially, puberty blockers are fully reversible: any youth who ultimately choose not to transition can discontinue blockers, and their original puberty will resume.
Puberty blockers are used in the treatment of appropriately diagnosed transgender youth, who wish to avoid developing undesired secondary sex characteristics of their assigned sex but are not yet old enough to commit to the permanent changes of hormone therapy. These medications, which are now administered at hospitals and gender clinics across the United States with the support of several major medical organizations, give an adolescent time to consider whether they want to go on to transition. Crucially, puberty blockers are fully reversible: any youth who ultimately choose not to transition can discontinue blockers, and their original puberty will resume.
But in recent years, some anti-trans advocates have claimed that puberty blockers should not be considered reversible, alleging that all youth who take blockers will inevitably go on to transition. Others have speculated that these medications may in some way affect the natural development of a child’s gender identity, making it more likely that they will transition when they otherwise would not have done so. Michelle Cretella, president of the transphobic American College of Pediatricians activist group, has asserted that “There are no cases in the scientific literature of gender-dysphoric children discontinuing blockers”, and Paul McHugh coauthored an article in The New Atlantis making this developmental argument at length:
The lack of data on gender dysphoria patients who have withdrawn from puberty-suppressing regimens and resumed normal development raises again the very important question of whether these treatments contribute to the persistence of gender dysphoria in patients who might otherwise have resolved their feelings of being the opposite sex. As noted above, most children who are diagnosed with gender dysphoria will eventually stop identifying as the opposite sex. The fact that cross-gender identification apparently persists for virtually all who undergo puberty suppression could indicate that these treatments increase the likelihood that the patients’ cross-gender identification will persist.
Such concerns are heavy on questions, but short on answers. As it turns out, these claims range from unsupported to outright false, and have already been extensively addressed in the literature on treatment of trans youth.
Cretella’s statement that there are “no cases in the scientific literature” of gender-dysphoric youth choosing to discontinue blockers is simply incorrect. Such cases have been reported in numerous publications:
- Tack et al. (2017) state that one male-assigned patient discontinued puberty-blocking treatment “because he no longer wanted to pursue sex reassignment”.
- Shumer, Nokoff, & Spack (2016) describe a case of a male-assigned patient who was given puberty blockers at age 12, but “developed a better understanding of their gender identity” during therapy and chose to stop taking blockers at 14, resuming normal male puberty.
- Lynch, Khandheria, & Meyer (2015) observe that one male-assigned patient and one female-assigned patient chose to discontinue treatment and resume living as their original gender.
- Khatchadourian, Amed, & Metzger (2014) note that a male-assigned patient “with undecided gender” discontinued taking blockers after 13 months “as he chose not to pursue transition”.
It is clearly not the case that there are no known instances of youth on blockers electing to resume their original puberty – such cases are indeed present in studies of gender-dysphoric youth undergoing this treatment. This is a particularly surprising oversight from a doctor who represents herself as the leader of a professional organization of pediatricians.
But could it still be the case that puberty-blocking treatment makes it more probable for these youth to retain their transgender identity, when experiencing their original puberty may have led some of them to adopt a cisgender identity? This too is unlikely. Clinicians do not administer blockers until these youth have reached Tanner stage 2 or 3 of their original puberty. A patient’s reaction to these changes – whether their gender-related distress begins to subside, or worsens with the arrival of some initial secondary sex characteristics of their assigned sex – is considered to be of value in clarifying the persistence of their gender dysphoria and whether they should continue to receive treatment (de Vries & Cohen-Kettenis, 2012):
If the eligibility criteria are met, gonadotropin releasing hormone analogues (GnRHa) to suppress puberty are prescribed when the youth has reached Tanner stage 2–3 of puberty; this means that puberty has just begun. The reason for this is that we assume that experiencing one’s own puberty is diagnostically useful because right at the onset of puberty it becomes clear whether the gender dysphoria will desist or persist.
Additionally, in interviews with 17 treatment teams specializing in gender-dysphoric youth, most did not endorse the concern that puberty blockers could interfere with development of gender identity (Vrouenraets, Fredriks, Hannema, Cohen-Kettenis, & de Vries, 2015):
However, although most informants agreed on the fact that treatment with puberty suppression indeed may change the way adolescents think about themselves, most of them did not think that puberty suppression inhibits the spontaneous formation of a gender identity that is congruent with the assigned gender after many years of having an incongruent gender identity.
These clinicians also observed that there already exists a “control group” of cisgender youth being given puberty blockers – those with precocious puberty – and that this treatment does not appear to have induced them to adopt a transgender identity:
Various endocrinologists made the comparison with precocious puberty; a medical condition in which puberty blockers have been used for many years, and no cases of GD have been described (at least to their knowledge).
Furthermore, the current evidence of the effects of puberty blockers on dysphoric adolescents’ brain function does not provide support to the notion that this treatment makes transgender identification more likely – a possibility that researchers explicitly acknowledge (Staphorsius et al., 2015):
In addition, we have shed some light on another concern that has been raised among clinicians: whether GnRHa treatment would push adolescents with GD in the direction of their experienced gender. We found no evidence for this and if anything, we found that puberty suppression even seemed to make some aspects of brain functioning more in accordance with the natal sex.
Criticisms of puberty-blocking treatment based on the claim that all treated youth go on to transition raise an important yet unanswered question: What proportion of these youth do they believe should be going on to transition? Rather than allegedly 100% continuing on a path toward transition, should this figure be only 95%? 80%? 50%? In considering these possibilities, the double bind of this criticism becomes clear: If only 80% of these youth progressed to transition, it could then be argued that clinicians have misdiagnosed 20% of these youth. If only 50% continued in their transition, then all the worse for the quality of clinicians’ diagnostic procedures.
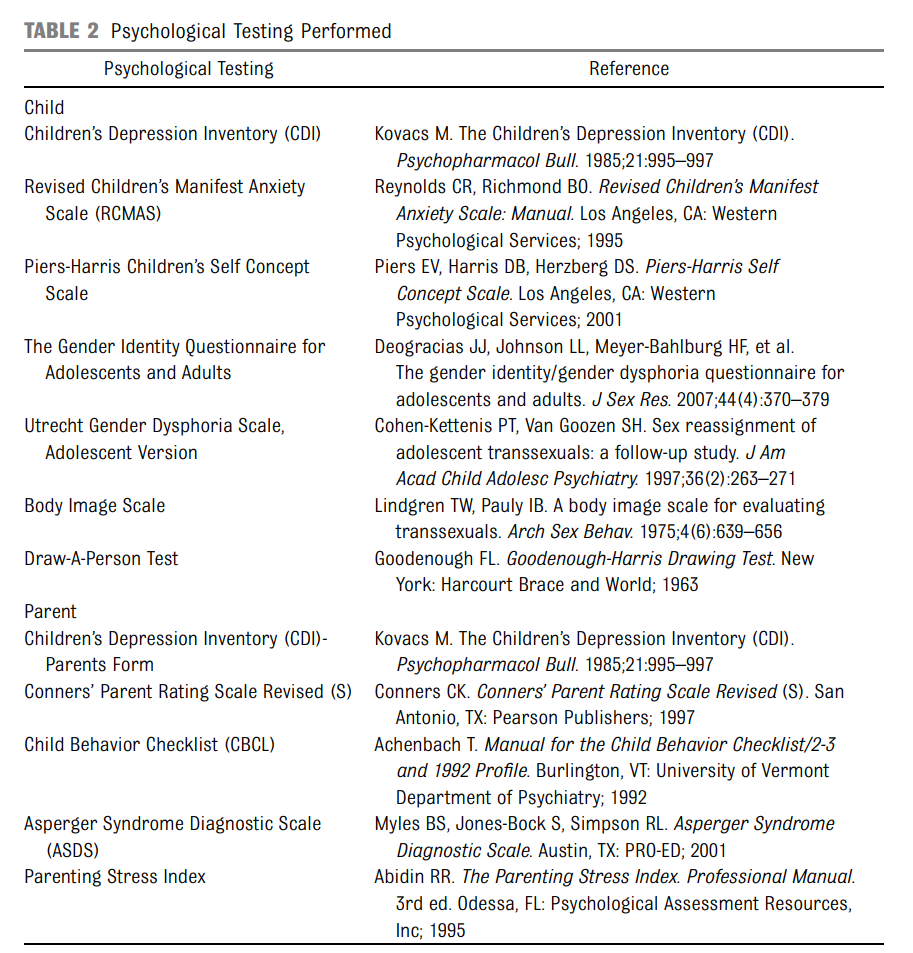
These critics do not seem to have allowed for the possibility that diagnostic screening of dysphoric youth could indeed be highly accurate in the vast majority of cases. Yet these diagnostic evaluations and criteria are very comprehensive and stringent, typically including a detailed interview of the child and parents as well as a battery of psychological tests (Spack et al., 2012):
Patients considered eligible for medical intervention (GnRH analogs and/or cross-sex hormones), first met with a psychologist, along with their parents, for a gender-identity–focused, structured, comprehensive clinical interview and psychometric testing (Table 2). The psychological protocol was adapted from the Adolescent Gender Identity Research network to assess the degree of gender dysphoria, coexisting psychiatric conditions, and psychosocial stability.
If anything, these criteria may be more strict than necessary, erring on the side of wrongly excluding some transgender youth rather than wrongly including some cisgender youth. This was made clear from the very beginning of the use of puberty blockers to treat dysphoric adolescents in the Netherlands (Smith, van Goozen, & Cohen-Kettenis, 2001):
Compared with adults, adolescents who start treatment before age 18 have additional criteria for treatment eligibility. As a consequence, those patients selected for early treatment are among the best-functioning transsexuals. … It appears to be possible to prevent false positives when following careful diagnostic procedures. … Although psychopathology may be the result rather than the underlying problem of the GID, SR may also be sought as a solution to nongender problems. Starting hormone treatment before adulthood should not be considered when many adverse factors operate simultaneously, despite the possibility that applicants may actually be transsexual. This is because it is more complicated to make an accurate diagnosis in problematic adolescents than in well-functioning adolescents, even for experienced multidisciplinary teams.
Transgender youth who receive treatment with puberty blockers are known to have improved mental health outcomes and better quality of life (Crall & Jackson, 2016), while those whose gender dysphoria remains untreated are at risk of depression, self-harm, and suicidal behavior (Radix & Silva, 2014). Is it theoretically possible that some marginal number of these youth may be otherwise-cisgender and are “nudged” by treatment over some borderline into transitioning? Perhaps. Is there currently any evidence of such a phenomenon at work? No – and there is certainly not sufficient evidence to justify withholding necessary treatment from youth who are suffering in the present on the off chance that we may hypothetically be able to eke out a few additional cis people from this group at some undetermined point in the future. ■
References
- Crall, C. S., & Jackson, R. K. (2016). Should psychiatrists prescribe gender-affirming hormone therapy to transgender adolescents? AMA Journal of Ethics, 18(11), 1086–1094.
- de Vries, A. L. C., & Cohen-Kettenis, P. T. (2012). Clinical management of gender dysphoria in children and adolescents: the Dutch approach. Journal of Homosexuality, 59(3), 301–320.
- Khatchadourian, K., Amed, S., & Metzger, D. L. (2014). Clinical management of youth with gender dysphoria in Vancouver. Journal of Pediatrics, 164(4), 906–911.
- Lynch, M. M., Khandheria, M. M., & Meyer, W. J. III. (2015). Retrospective study of the management of childhood and adolescent gender identity disorder using medroxyprogesterone acetate. International Journal of Transgenderism, 16, 201–208.
- Radix, A., & Silva, M. (2014). Beyond the guidelines: challenges, controversies, and unanswered questions. Pediatric Annals, 43(6), e145–e150.
- Shumer, D. E., Nokoff, N. J., & Spack, N. P. (2016). Advances in the care of transgender children and adolescents. Advances in Pediatrics, 63(1), 79–102.
- Smith, Y. L. S., van Goozen, S. H. M., & Cohen-Kettenis, P. T. (2001). Adolescents with gender identity disorder who were accepted or rejected for sex reassignment surgery: a prospective follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry, 40(4), 472–481.
- Spack, N. P., Edwards-Leeper, L., Feldman, H. A., Leibowitz, S., Mandel, F., Diamond, D. A., & Vance, S. R. (2012). Children and adolescents with gender identity disorder referred to a pediatric medical center. Pediatrics, 129(3), 418–425.
- Staphorsius, A. S., Kreukels, B. P. C., Cohen-Kettenis, P. T., Veltman, D. J., Burke, S. M., Schagen, S. E. E., . . . Bakker, J. (2015). Puberty suppression and executive functioning: an fMRI-study in adolescents with gender dysphoria. Psychoneuroendocrinology, 56, 190–199.
- Tack, L. J. W., Heyse, R., Craen, M., Dhondt, K., Vanden Bossche, H., Laridaen, J., & Cools, M. (2017). Consecutive cyproterone acetate and estradiol treatment in late-pubertal transgender female adolescents. Journal of Sexual Medicine, 14(5), 747–757.
- Vrouenraets, L. J. J. J., Fredriks, A. M., Hannema, S. E., Cohen-Kettenis, P. T., & de Vries, M. C. (2015). Early medical treatment of children and adolescents with gender dysphoria: an empirical ethical study. Journal of Adolescent Health, 57(4), 367–373.




Pingback: When “desisters” aren’t: De-desistance in childhood and adolescent gender dysphoria | Gender Analysis