 Collaboration between the transgender community and health researchers plays an essential role in ensuring that our population’s knowledge and interests are acknowledged and represented in medicine. When researchers neglect to reach out and utilize the community’s collected experiences and shared knowledge, it’s easy for them to overlook significant issues that are widely recognized among trans people but make almost no appearance in medical literature. For instance, consider the phenomenon of chronic depersonalization disorder in trans people, which we’ve frequently described as intense and unremitting before starting HRT, and suddenly disappearing once we’re on HRT. Yet the specific symptoms of depersonalization among trans people have only barely been studied in medical publications. Conversely, trans people often find themselves without access to the language, to the term depersonalization, to describe these symptoms as what they are.
Collaboration between the transgender community and health researchers plays an essential role in ensuring that our population’s knowledge and interests are acknowledged and represented in medicine. When researchers neglect to reach out and utilize the community’s collected experiences and shared knowledge, it’s easy for them to overlook significant issues that are widely recognized among trans people but make almost no appearance in medical literature. For instance, consider the phenomenon of chronic depersonalization disorder in trans people, which we’ve frequently described as intense and unremitting before starting HRT, and suddenly disappearing once we’re on HRT. Yet the specific symptoms of depersonalization among trans people have only barely been studied in medical publications. Conversely, trans people often find themselves without access to the language, to the term depersonalization, to describe these symptoms as what they are.
Better communication between the trans and medical communities can be mutually enriching, with medical professionals becoming aware of key issues among the trans population that they may have overlooked, and trans people being able to tap into the resources of medical researchers to investigate and more rigorously clarify various aspects of our health. And one such collaboration has recently shed light on a previously unstudied issue: the emergence of new abdomino-pelvic pain in trans men and transmasculine people after beginning treatment with testosterone.
After observing this phenomenon commonly occurring among their transmasculine patients receiving testosterone, Grimstad, Boskey, & Grey (2020) conducted a community survey on these symptoms in cooperation with The Union, an organization which describes themselves as “a support, social and resource group that caters to the female-to-male, transgender community” in the Kansas City metropolitan area. Working with members of The Union, the authors crafted a survey on these symptoms and reached 127 transmasculine people in the community who reported “endorsed ‘new-onset discomfort in [their] abdomen and/or pelvis since [their] initiation’ of testosterone therapy”. These results helped elucidate the timing of the onset of this pain, its frequency, what events preceded it, the location and specific feeling(s) of the pain, and what if anything led to its resolution.
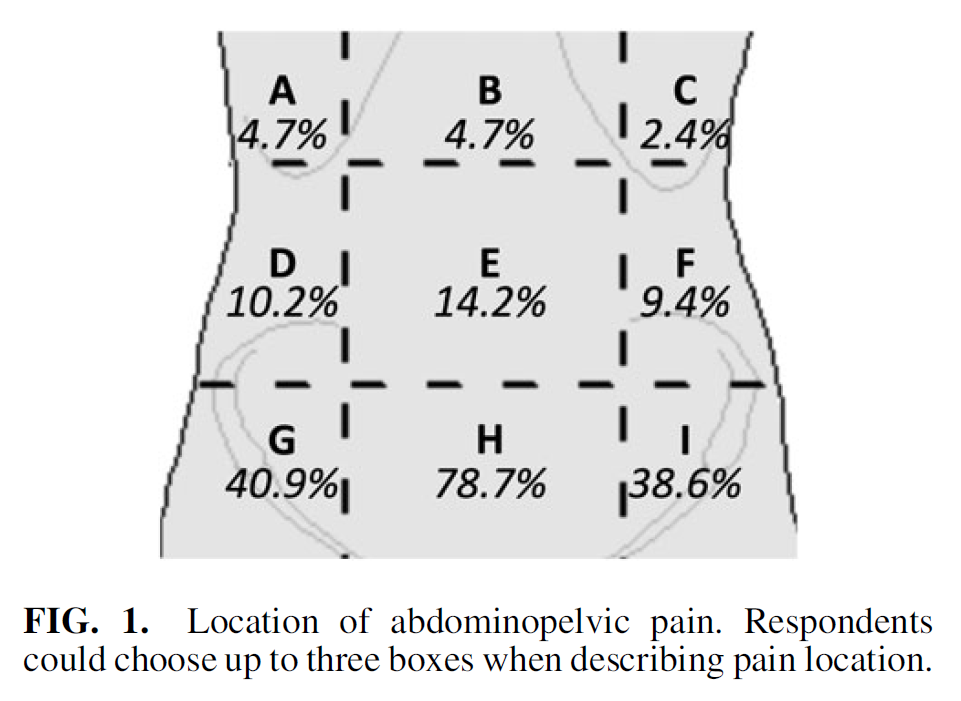
These respondents reported that their abdomino-pelvic pain began at a median of one year after starting testosterone, albeit with a wide range, from one month to 20 years. Their pain was most frequently reported as occurring in the suprapubic region:
75.6% of respondents described the pain as “cramping”, along with 41.7% describing it as “sharp” and 38.6% as “achy” (respondents could select more than one option). Notably, those who localized their pain to the suprapubic region (region H) were much more likely than other respondents to state that this was a cramping pain. 79.5% said the pain was intermittent, with a roughly even division between those who usually experienced pain during the day or the night. Of the 13 respondents who reported that the pain was cyclical – neither intermittent nor constant – 84.6% said that this was monthly. When listing factors that appeared to precede a worsening of the pain, 59.1% said that it occurred spontaneously, although 46.4% reported sexual intercourse as bringing on or worsening the pain, and 14.2% reported that eating was a cause. Only 9 respondents had received a diagnosis for the cause of the pain, and the specific diagnosis was only known for 2 respondents, who reported interstitial cystitis (a painful bladder condition) and adenomyosis (the growth of endometrial tissue into the muscular wall of the uterus).
Only 22.8% said that medications helped to improve the pain, while 28 respondents said that a surgery or treatment permanently resolved the pain; all 28 reported that this surgery was a hysterectomy. However, 10.2% of all respondents had neither a uterus nor ovaries yet still experienced ongoing abdomino-pelvic pain.
Based on these characterizations of the pain experienced by transmasculine people on testosterone, the authors recognize that the cause of this condition is not definitely known, but generate several hypotheses for the likely origins and mechanisms of this pain:
The combination of the suprapubic location of most of the reported pain with the effectiveness of hysterectomy as a treatment is suggestive of a reproductive organ etiology. . . . No clear mechanism exists by which androgen-induced changes in the ovaries would cause pain; therefore, a uterine etiology is more plausible as an explanation for hysterectomy as curative in these instances . . . . Uterine atrophy is unlikely to be a cause as this is a common finding in postmenopausal persons but has not been linked to increased pain. However, given persistent endometrial activity in some trans-masculine persons, prostaglandin changes and uterine hypoperfusion, which both play a role in dysmenorrhea and occur in reproductive age uteri, may contribute to new-onset pain. Removal of the uterus through hysterectomy would theoretically remove these localized sources of pain and could be the reason that 28 respondents found hysterectomy curative.
Going forward, the authors state that “with future research we would like to directly assess hormonal contraceptive and nonsteroidal antiinflammatory drug use, as both have previously been shown to decrease prostaglandins in the uterus—a potential etiology for abdominopelvic pain”, along with “ascertaining the impact of testosterone type, dosing, and serum levels on abdominopelvic pain, understanding the effects of testosterone on prostaglandin activity in the endometrium, and evaluating both successful and unsuccessful therapies”. This study has provided a valuable starting point, offering acknowledgment from the medical field – spurred by the trans community – that many trans men do experience this abdomino-pelvic pain after starting testosterone, and calling for further investigation into the causes and potential treatment of this pain. ■




One Response to Open questions: Trans men and transmasculine people can experience abdominal and pelvic pain after starting testosterone